
home health nurse responsibilities pdf
Explore the key duties and requirements for home health nurses. Download our detailed PDF guide now!
Home health nursing involves providing skilled medical care to patients in their homes, focusing on recovery, disease management, and improving quality of life.

Key Responsibilities of Home Health Nurses
Home health nurses provide skilled care, including patient assessments, administering medications, wound care, education, and monitoring progress to ensure optimal patient outcomes in their homes.
- Conduct comprehensive patient evaluations.
- Administer medications and treatments as prescribed.
- Provide wound care and manage chronic conditions.
- Educate patients and families on care practices.
- Monitor and report changes in patient status.
2.1 Patient Assessment and Evaluation
Home health nurses conduct thorough patient assessments to identify medical, emotional, and environmental needs. This involves evaluating medical history, performing physical exams, and reviewing diagnostic data.
- Evaluate patients’ physical and mental condition to develop personalized care plans.
- Identify risk factors, such as falls or infections, to prevent complications.
- Assess home safety and recommend modifications for a safe living environment.
- Monitor vital signs and document changes in health status.
- Collaborate with healthcare teams to update care plans based on patient progress.
This process ensures tailored interventions, promoting optimal recovery and well-being in the home setting.
2.2 Administering Medications and Treatments
Home health nurses play a crucial role in administering medications and treatments tailored to patients’ specific needs. This ensures adherence to prescribed plans and promotes recovery.
- Administer oral, intravenous, and injectable medications as directed by physicians.
- Monitor patients for adverse reactions and adjust treatments accordingly.
- Perform procedures like IV therapy, wound care, and catheter management.
- Educate patients and families on proper medication use and treatment protocols.
- Document administration details and patient responses accurately.
These tasks ensure safe and effective care, improving patient outcomes in the home setting while maintaining compliance with healthcare standards.
2.3 Wound Care and Management
Home health nurses specialize in wound care, providing essential treatment to promote healing, prevent infection, and improve patient comfort.
- Assess wound size, depth, and tissue type to develop personalized care plans.
- Clean, debride, and dress wounds using sterile techniques and advanced products.
- Monitor for signs of infection, such as redness or purulent drainage, and report changes.
- Educate patients and caregivers on proper wound care and prevention strategies.
- Utilize therapies like negative pressure wound therapy or compression wraps as needed.
- Document progress and adjust treatment plans to ensure optimal healing outcomes.
Effective wound management by home health nurses enhances recovery, reduces hospital readmissions, and improves overall patient well-being.
2.4 Patient and Family Education
Patient and family education is a cornerstone of home health nursing, empowering individuals to manage their care effectively and improve health outcomes.
- Home health nurses teach patients and caregivers about medications, treatments, and disease management.
- They demonstrate how to use medical equipment and perform daily care tasks safely.
- Education includes wound care, nutrition, and mobility techniques to prevent complications.
- Nurses provide resources and guidance to help families support their loved ones.
- They ensure understanding of care plans and address any concerns or questions.
- Collaborating with healthcare teams, nurses tailor education to meet individual needs.
By educating patients and families, home health nurses promote independence, adherence to treatment, and overall well-being.
2.5 Monitoring and Reporting Progress
Monitoring and reporting patient progress is a critical responsibility of home health nurses, ensuring timely adjustments to care plans and optimal outcomes.
- Nurses conduct regular assessments to track patients’ physical, emotional, and functional changes.
- They document progress, identifying improvements or declines in condition.
- Accurate records are maintained to inform the healthcare team and guide decision-making.
- Reports are shared with physicians and other providers to update treatment plans.
- Nurses also communicate findings to patients and families, keeping them informed.
- This continuous oversight helps address potential issues early and enhances care quality.
By closely monitoring and reporting progress, home health nurses ensure personalized, effective care tailored to each patient’s evolving needs.
Required Skills and Qualifications
Home health nurses must possess specific skills and qualifications to deliver high-quality patient care in diverse home settings.
- A valid Registered Nurse (RN) or Licensed Practical Nurse (LPN) license is essential.
- At least 2 years of experience in healthcare, preferably in home health or a related field, is often required.
- Strong communication skills are critical for coordinating care and interacting with patients, families, and healthcare teams.
- Critical thinking and problem-solving abilities are necessary for managing complex patient conditions.
- Ability to work independently and manage time effectively is vital due to the autonomous nature of home health nursing.
- Physical stamina is required to handle tasks like wound care and patient mobility assistance.
- Compassion and emotional resilience are crucial for supporting patients and their families.
These qualifications ensure home health nurses can provide skilled, patient-centered care in a variety of home-based settings.
Work Environment and Setting
Home health nurses operate in a unique and dynamic environment, primarily providing care in patients’ homes, which can vary significantly in location and condition.
- The setting often requires travel between multiple patient locations, adapting to diverse home environments, and managing unpredictable situations.
- Home health nurses care for patients with chronic illnesses, disabilities, or those recovering from surgery, often working independently with minimal direct supervision.
- The role demands strong clinical judgment, as decisions must be made autonomously, ensuring patient safety and effective care delivery.
- Collaboration with other healthcare professionals, such as physicians and therapists, is essential to coordinate comprehensive patient care plans.
- The work environment also involves documentation and reporting, with nurses required to maintain detailed records of patient progress and treatment outcomes.
This setting requires adaptability, resilience, and a commitment to delivering high-quality care in non-traditional healthcare environments.

Benefits of Being a Home Health Nurse
Being a home health nurse offers numerous rewards, including the opportunity to make a meaningful impact on patients’ lives in their own homes.
- Home health nurses experience high job satisfaction due to the ability to build strong patient relationships and witness significant progress in recovery.
- The role provides flexibility, with varying schedules and the potential for part-time or per-diem opportunities, allowing for better work-life balance.
- Professionals in this field gain diverse clinical experience, treating a wide range of conditions and enhancing their critical thinking and problem-solving skills.
- Home health nursing fosters autonomy, as nurses often work independently, making decisions that directly impact patient care outcomes;
- The emotional rewards of helping patients maintain independence and comfort in their homes contribute to a fulfilling career path.
These benefits make home health nursing a rewarding and challenging profession for those passionate about patient-centered care.

Challenges Faced by Home Health Nurses
Home health nurses encounter unique challenges that require adaptability and resilience. Working independently in diverse patient settings can lead to feelings of isolation and increased responsibility for decision-making. Managing varying patient conditions, from acute care to chronic disease management, demands strong clinical skills and critical thinking. Additionally, navigating unpredictable schedules, travel demands, and time management between visits can be physically and emotionally taxing. Safety concerns, such as visiting unfamiliar neighborhoods, also pose risks. Emotional challenges arise from exposure to end-of-life care and high-stress situations. Moreover, the need to balance patient care with administrative duties, such as documentation, adds to the workload. These challenges highlight the complexity and demands of home health nursing, requiring nurses to be resourceful and compassionate in their practice.
Documentation and Reporting Responsibilities
Home health nurses are responsible for maintaining accurate and detailed records of patient care. This includes documenting medical histories, treatment plans, and progress during visits. Timely and precise reporting ensures compliance with healthcare regulations and agency policies. Nurses must also communicate effectively with interdisciplinary teams through written reports, fostering continuity of care. Additionally, they prepare and update care plans, reflecting patient goals and outcomes. Accurate documentation is crucial for billing, legal purposes, and future reference. Home health nurses often use electronic health records (EHRs) to streamline data entry and improve accessibility. Ensuring confidentiality and adherence to HIPAA guidelines is paramount. This systematic approach to documentation supports high-quality patient care and accountability in home health settings, making it a cornerstone of their responsibilities.

Patient Care Coordination
Home health nurses play a vital role in coordinating patient care, ensuring seamless communication and collaboration among healthcare providers. They work closely with physicians, therapists, and other specialists to develop and implement personalized care plans. Coordinating services includes scheduling visits, managing medical equipment, and arranging community resources. Nurses assess patient needs, prioritize interventions, and monitor progress to achieve optimal outcomes. Effective communication with patients, families, and caregivers is essential to address concerns and adapt care plans as needed. Home health nurses also facilitate transitions between care settings, such as hospitals to home, to ensure continuity of care. By acting as a liaison, they help patients navigate the healthcare system, making care more accessible and efficient. This role requires strong organizational, interpersonal, and problem-solving skills to deliver coordinated, patient-centered care.

Legal and Ethical Considerations
Home health nurses must adhere to legal and ethical standards to ensure patient rights and safety. They are required to maintain patient confidentiality and uphold HIPAA regulations, protecting sensitive health information. Ethical dilemmas may arise, such as end-of-life decisions or conflicts between patient autonomy and family wishes. Nurses must practice within their scope of licensure and follow state and federal laws governing home healthcare. They are also responsible for reporting abuse or neglect and ensuring informed consent for treatments. Ethical considerations include respecting patient preferences, avoiding harm, and providing compassionate care. Legal documentation and accurate record-keeping are crucial to support ethical practice and comply with regulatory requirements. Staying informed about legal updates and ethical guidelines is essential for home health nurses to deliver care responsibly and with integrity.
Tools and Resources for Home Health Nurses
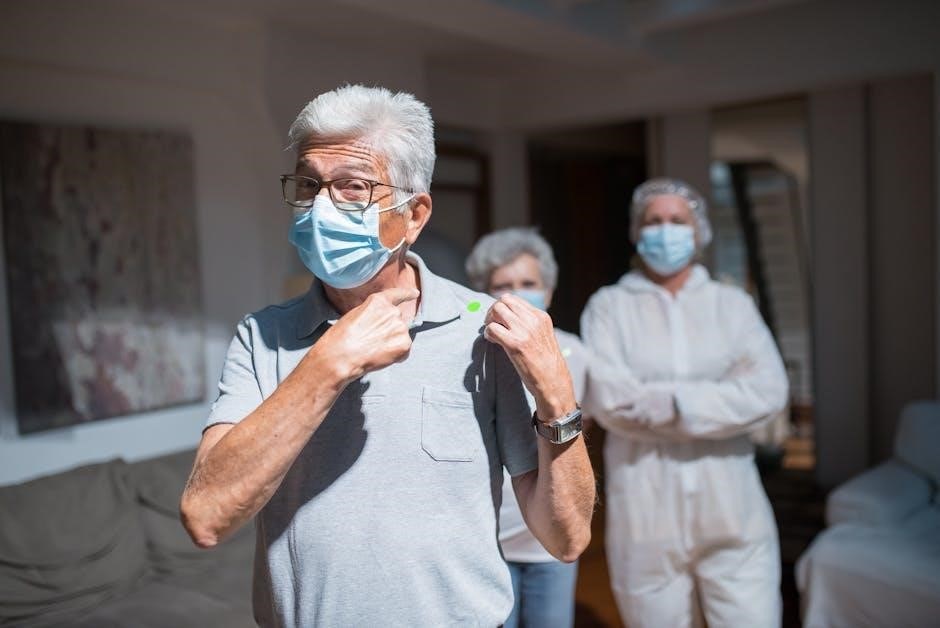
Home health nurses rely on various tools and resources to deliver effective care. Electronic health records (EHRs) and telehealth platforms enable remote patient monitoring and communication. Portable medical equipment, such as blood pressure monitors and wound care supplies, are essential for patient assessments. Additionally, home health nurses utilize care coordination software to manage patient schedules and track progress. Educational resources, like clinical guidelines and training programs, help nurses stay updated on best practices. Professional organizations, such as the National Association for Home Care & Hospice, provide support and advocacy. Access to reliable transportation and personal protective equipment (PPE) is also critical for safe and efficient care delivery in diverse home settings.